In response to the COVID-19 pandemic, the American Heart Association and collaborating organizations, including the American Academy of Pediatrics, the American Association for Respiratory Care, the Society of Critical Care Anesthesiologists and the American Society of Anesthesiologists, continue to provide interim guidance to address the latest scientific research related to the SARS-CoV-2 virus, particularly the Delta and Omicron variants. The updated “2022 Interim Guidance to Health Care Professionals for Basic and Advanced Cardiac Life Support in Adults, Children, and Neonates With Suspected or Confirmed COVID-19 addresses the emergence of COVID-19 variants that are more transmissible than previous strains.
“Based on evolving epidemiology reports and emerging science, the volunteer committee comprised of more than 40 global resuscitation experts has issued new guidance for the resuscitation of patients with suspected or confirmed COVID-19. This guidance also reflects the recommendations issued recently from both the World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention (CDC).”
Comilla Sasson, M.D., Ph.D., FAHA, practicing emergency medicine physician and vice president for science & innovation for emergency cardiovascular care, American Heart Association

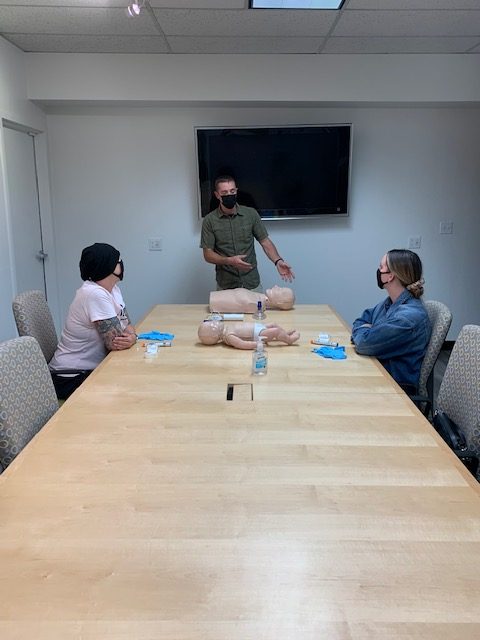
Most significantly, due to new, more highly contagious variants of the SARS-CoV-2 virus, the guidance emphasizes the need for PPE, including respirators, gowns, gloves and eye protection. In the event initial responders are not already wearing appropriate PPE, they should immediately put on PPE and then begin CPR. As the science surrounding COVID-19 and variants evolves, health care professionals should continue to follow the most-up-to-date recommendations from the WHO, CDC and their regional health authorities and local institutions.
“Health care professionals are paramount to the health of communities around the world, especially during a pandemic, and they should be protected while performing health care procedures including resuscitation,” said Dianne Atkins, M.D., FAAP, volunteer chair of the American Heart Association Emergency Cardiovascular Care Committee, a pediatric cardiologist and lead author of the new interim guidance. “Protecting the health and safety of health care professionals remains critical and includes ensuring the recommended personal protective equipment is available and that health care professionals are trained to use it properly.”
Additional updates in the guidance include:
- Incorporating the most recent CDC and WHO guidance: All healthcare providers should wear a respirator (e.g., N95) along with other PPE (gown, gloves, and eye protection) for patients with suspected or confirmed COVID-19 infection, when performing aerosol-generating procedures (AGP)s or in a setting where such procedures are regularly performed. This includes wearing appropriate PPE (including a respirator) before performing the components of resuscitation that are aerosol-generating, which include but are not limited to chest compressions, defibrillation, bag-mask ventilation, intubation or positive-pressure ventilation.
2. Reinforcing resuscitation best practices: Cardiac arrest survival rates have decreased dramatically during the COVID-19 pandemic. Out of hospital cardiac arrest survival in 2020 also declined in regions/timeframes that did and did not have significant COVID infection rates. The reasons for this decline are both unclear and complex. Cardiac arrest survival is dependent on early initiation of CPR, including chest compressions as soon as it is safely possible. Patients with confirmed or suspected COVID-19 should receive the best resuscitative efforts possible.
3. Ensuring adequate PPE supply: At this time, all healthcare providers should be following appropriate precautions and should have access to PPE in all clinical settings, regardless of the potential of encountering resuscitation events. Effective use of PPE is critical for the safety of healthcare providers performing resuscitations. Healthcare organizations should continue to secure appropriate PPE as available, ensure training regarding appropriate application and use of PPE, reinforce effective use of PPE, and create systems so that health care providers have immediate access to appropriate PPE when emergency care is required.
As the COVID-19 pandemic persists and new variants arise, the American Heart Association with its collaborating professional organizations will continue to provide the most up-to-date, evidence-based guidance on resuscitation and supporting the health care professionals that provide these life-saving procedures such as CPR.
American Heart Association guidance articles promote greater awareness about cardiovascular diseases and stroke issues and help facilitate informed health care decisions. Scientific statements and guidance documents outline what is currently known about a topic and what areas need additional research. While scientific statements and guidance documents inform the development of formal guidelines, they do not make treatment recommendations. American Heart Association guidelines provide the Association’s official clinical practice recommendations.