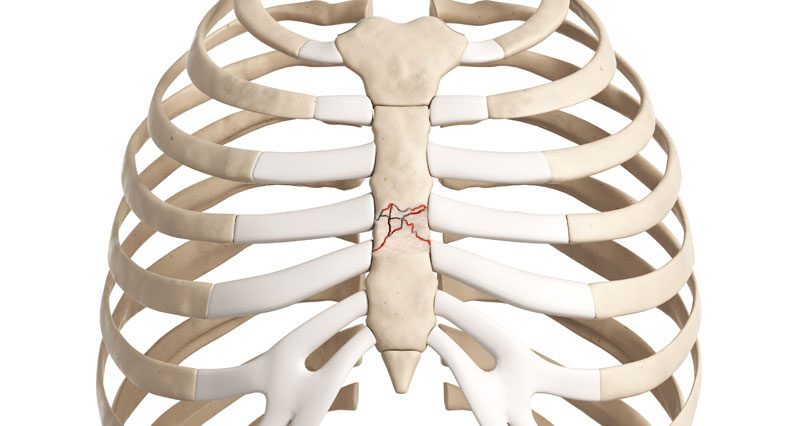
Broken Ribs During CPR – Being CPR Certified is different to actually apply in real life situation. One of the biggest concerns in performing CPR for the first time is whether or not you will accidentally break a patient ribs or other bones. Applying pressure to the rib area while performing the necessary chest compressions can can cause injuries. Because of this risk, many students learning CPR hesitate to apply their CPR Skills.
In order for CPR to be effective (in adult patients), chest compressions need to be performed at a depth of approximately 2 inches (5.08 cm) in depth. Shallow compressions will not sufficiently circulate the blood around the body. Compressing the human chest by that much, requires a significant amount of force. Giving this amount of force, we can easily understand how and why ribs may break in the process of performing CPR. Approximately 30% of patients receiving CPR suffer rib fractures or bone breaks. Those numbers may actually be higher.
The study analyzed autopsy data from more than 2,000 patients who had received CPR for cardiac
- 86% of men and 91% of women presented with skeletal chest injuries
- 59% of those men and 79% of those women had fractures of the sternum
- 77% of those men and 85% of those women had fractures of the ribs
- 33% of those men and 12% of those women had sternocostal separation
As you can see, a significant portion of patients had suffered from some type of Broken Ribs During CPR or fracture.
When you perform resuscitation on a patient, high chances of injury may occur.
Who is most at risk of breaking the ribs during CPR?

Base on the data provided from the above referenced study shows that women are more likely than men to experience injuries or Broken Ribs During CPR.
The study also found that older patients tend to be more at risk of CPR-related injury than those who are younger.
Also, the presence of certain existing health conditions, such as osteoporosis, which causes a weakening of the bones, can also increase the risk of skeletal injury.
Patients who are physically large, particularly those who are fat are much less likely to suffer broken bones due to CPR than those with smaller frames.
Another study performed in Korea revealed that patients receiving CPR from a bystander are more likely to suffer chest injuries than individuals who receive CPR from a trained professional, such as a doctor or a paramedic.
So, the good news is, if you are properly educated on how to correctly deliver effective chest compressions, your risk of injuring someone in the process may be lower.
Risk of injury also goes up based on the size and strength of the individual performing CPR as well.
Generally speaking, men tend to cause more rib fractures and breaks due to the fact that they tend to have more upper body strength than women. Of course, this is not always the caseb
What should you do if you hear (or feel) a bone crack during CPR?
In the event that a person on whom you are performing CPR experience a broken or fractured bone, you may hear a cracking sound.
At the very least, you’ll probably feel something crack or give way under your hands.
This is not always indicate of an actual bone break.
The initial sound or feeling of cracking can often be attributed to the cartilage in the ribs or sternum breaking, as opposed to the ribs themselves.
it is not advisable to stop performing CPR even if you hear a cracking sound or think you feel a rib break.
It is true that broken bones can be painful and may extend a person’s recovery time, stopping resuscitation efforts could result death into patient.
A patient who survived as a result of CPR would be happy even the patient suffer a broken bone. Thanks to the resuscitator’s quick response.
Don’t be afraid to perform CPR

You should never should never be afraid of breaking someone’s ribs or causing other injuries during the life-saving efforts.
Broken bones and injuries heal, but death is forever.
Most states have laws that protect people who deliver CPR in good faith.
That means even in the unlikely event that someone were to try and sue, you would be protected.
The fact is, CPR is a vigorous and sometimes brutal procedure.
There will always be a risk that the person who receive CPR become injured during the process.
However, if the person you assist is lucky enough to survive, you can expect a heartfelt thank you for the broken ribs.