The Reason Why Strokes Often Happen in the Bathroom.

Before moving ahead; we must understand the basic difference between these events;
Heart Attack: It occurs when blood flow to the heart is blocked. It is a circulatory problem. A heart attack could be due to blockage of an artery that supplies blood to an area of your heart.
Cardiac Arrest: It occurs when the heart malfunctions and stops beating unexpectedly. It is an electrical problem causing the irregular heartbeat. This prevents the heart from pumping the blood to the other parts of the body including the brain. As the muscles won’t expand and contract, the blood won’t flow.
These two conditions are linked. A sudden cardiac arrest can happen after a heart attack.
Stroke: When blood flows to an area of the brain cut-off. Hence, brain cells deprived of the oxygen and glucose needed to survive.
Why do they happen in the bathroom often?
The study has shown that there is a rapid increase in bathing death accidents. It is mentioned that the causes of death while bathing is primarily cardiovascular diseases followed by cerebrovascular and respiratory diseases.
Toilet Strain
Heart attacks which occur during defecation are, in many cases, the result of using the (unnatural) sitting posture for waste elimination. Excessive strain during defecation adversely affects the cardiovascular system. Results in syncope or death. Syncope is a temporary loss of consciousness usually related to insufficient blood flow to the heart. Straining on the stool may reduce your blood pressure. This leads to an insufficient supply of blood to the heart.
Use of a sitting toilet triggers the risk more than a squatting toilet as it requires more strain. It may trigger cardiac arrest in the bathroom often.
Abrupt changes in Blood pressure
For high blood pressure people, sequenced bathing, the temperature of water and season should be on the count, as mentioned above. Sudden cold water exposure increases sympathetic tone which further causing a rapid fall in skin temperature. It leads to rising blood pressure.
Early to rise!
Morning may be the most dangerous time of the day for older people with high blood pressure. Usually, we use the toilet and take a bath in the morning. The onset of events are more in late mornings from 8 am to 11 am, study says.
Bathing is suspected of causing abrupt changes in blood pressure that induce ischemia in the cerebral blood vessels. This could drive a stroke or heart attack or a cardiac arrest in the bathroom or toilet.
A person with a history of high blood pressure or myocardial infarction must be careful about bathing. The difference in temperature in the bathtub and body could cause abrupt changes in blood pressure.
No sequenced bath or shower
“While bathing or showering, do not wet the head and hair first. This is the wrong sequence.” Writes a professor at UiTM National Sports Board. We tend to take bath by letting go shower or bucket water on our head directly. It causes the body to adjust its temperature too quickly because we are warm-blooded. It may generate pressure and cause artery or capillary breakage.
Sequenced bathing is very important to avoid such incidences. Start with wetting your legs and up to your head gently. Frequently, incidences of stroke or heart attack or cardiac arrest in the bathroom happen more in winter than in summer. Water temperature matters a lot while bathing.
In the nutshell
Events like stroke/Heart Attack/Cardiac arrest can happen to anybody anywhere at any time. It’s good that everyone is familiar with the signs of heart attack, stroke and cardiac arrest and act on time when such a situation occur. Most importantly a right lifestyle is the best way to stay away from a heart attack and stroke!
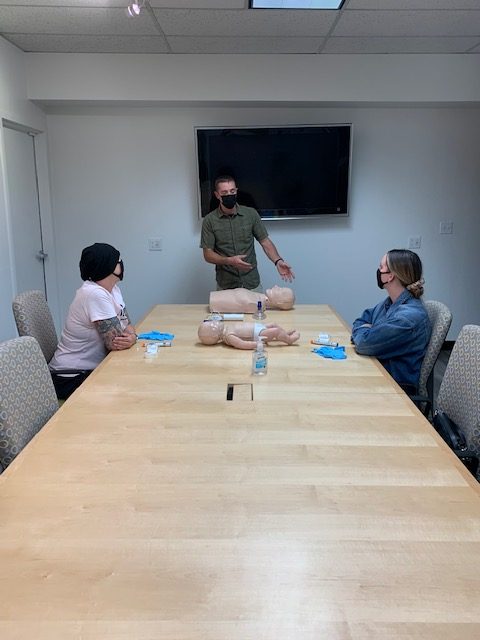
For Safety Reason, You Should Learn CPR.
Cardiac arrest and stroke can happen more often than we think. It happens to anyone at any time, yet most Americans do not know how to perform CPR. When done properly and immediately, CPR has proven to save lives.
The American Heart Association (AHA) has a vast network of instructor’s that train millions of people globally each year with international training centers in more than 100 countries and over 300 translated products. In spite of global efforts and the use of CPR since 1740’s, a high percentage of Americans don’t know how to act or respond during an emergency situation.

Many people say that they do not have time to learn or don’t want to learn CPR.
This mindset may be attributed to the fact that we never fathom the emergency being one of our own.
We do not realize that every single day we are at risk being involved in activities that can lead to an emergency whether work related or driving down the road. A healthy individual may receive an unexpected blow to the chest that causes the heart to stop beating.
A three-year-old toddler may acquire an occluded airway from the thick paste of peanut butter that has stuck to the throat.
What about the little boy who collapsed on the school bus in Atlanta, Georgia on May 7, 2019? Luckily for him he was revived by 7-year-old Janea who recognized an emergency situation had occurred and her immediate actions would help save his life. If you think a young child cannot perform CPR, think again.
During summer, it tends to peak a high rate of water safety incidents.
The Fox 26 News in Houston reported that Texas is number one in the states for drowning incidents.
This is not just a Texas concern, this is every state and every county concern, yet there are several parents and caregivers who have not been trained or a significant amount of time has lapsed since their last CPR training.
Adults and caregivers should refresh their infant, child CPR yearly, especially right before summers when water is involved.
70% of sudden cardiac arrest happens in public places or at home.
Failure to ACT immediately in a cardiac emergency leads to death. When effective bystander CPR is provided an individual’s chance of survival is doubled and even tripled.
Be a keeper for your community, an advocate for your family, and an effective first responder for all who will need you.
Be Trained To act immediately during an emergency situation. Always Remember, EVERY SECOND COUNTS!
New CPR guidance issue by experts addressing the highly contagious Delta and Omicron variants of SARS-CoV-2
In response to the COVID-19 pandemic, the American Heart Association and collaborating organizations, including the American Academy of Pediatrics, the American Association for Respiratory Care, the Society of Critical Care Anesthesiologists and the American Society of Anesthesiologists, continue to provide interim guidance to address the latest scientific research related to the SARS-CoV-2 virus, particularly the Delta and Omicron variants. The updated “2022 Interim Guidance to Health Care Professionals for Basic and Advanced Cardiac Life Support in Adults, Children, and Neonates With Suspected or Confirmed COVID-19 addresses the emergence of COVID-19 variants that are more transmissible than previous strains.
“Based on evolving epidemiology reports and emerging science, the volunteer committee comprised of more than 40 global resuscitation experts has issued new guidance for the resuscitation of patients with suspected or confirmed COVID-19. This guidance also reflects the recommendations issued recently from both the World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention (CDC).”
Comilla Sasson, M.D., Ph.D., FAHA, practicing emergency medicine physician and vice president for science & innovation for emergency cardiovascular care, American Heart Association

Most significantly, due to new, more highly contagious variants of the SARS-CoV-2 virus, the guidance emphasizes the need for PPE, including respirators, gowns, gloves and eye protection. In the event initial responders are not already wearing appropriate PPE, they should immediately put on PPE and then begin CPR. As the science surrounding COVID-19 and variants evolves, health care professionals should continue to follow the most-up-to-date recommendations from the WHO, CDC and their regional health authorities and local institutions.
“Health care professionals are paramount to the health of communities around the world, especially during a pandemic, and they should be protected while performing health care procedures including resuscitation,” said Dianne Atkins, M.D., FAAP, volunteer chair of the American Heart Association Emergency Cardiovascular Care Committee, a pediatric cardiologist and lead author of the new interim guidance. “Protecting the health and safety of health care professionals remains critical and includes ensuring the recommended personal protective equipment is available and that health care professionals are trained to use it properly.”
Additional updates in the guidance include:
- Incorporating the most recent CDC and WHO guidance: All healthcare providers should wear a respirator (e.g., N95) along with other PPE (gown, gloves, and eye protection) for patients with suspected or confirmed COVID-19 infection, when performing aerosol-generating procedures (AGP)s or in a setting where such procedures are regularly performed. This includes wearing appropriate PPE (including a respirator) before performing the components of resuscitation that are aerosol-generating, which include but are not limited to chest compressions, defibrillation, bag-mask ventilation, intubation or positive-pressure ventilation.
2. Reinforcing resuscitation best practices: Cardiac arrest survival rates have decreased dramatically during the COVID-19 pandemic. Out of hospital cardiac arrest survival in 2020 also declined in regions/timeframes that did and did not have significant COVID infection rates. The reasons for this decline are both unclear and complex. Cardiac arrest survival is dependent on early initiation of CPR, including chest compressions as soon as it is safely possible. Patients with confirmed or suspected COVID-19 should receive the best resuscitative efforts possible.
3. Ensuring adequate PPE supply: At this time, all healthcare providers should be following appropriate precautions and should have access to PPE in all clinical settings, regardless of the potential of encountering resuscitation events. Effective use of PPE is critical for the safety of healthcare providers performing resuscitations. Healthcare organizations should continue to secure appropriate PPE as available, ensure training regarding appropriate application and use of PPE, reinforce effective use of PPE, and create systems so that health care providers have immediate access to appropriate PPE when emergency care is required.
As the COVID-19 pandemic persists and new variants arise, the American Heart Association with its collaborating professional organizations will continue to provide the most up-to-date, evidence-based guidance on resuscitation and supporting the health care professionals that provide these life-saving procedures such as CPR.
American Heart Association guidance articles promote greater awareness about cardiovascular diseases and stroke issues and help facilitate informed health care decisions. Scientific statements and guidance documents outline what is currently known about a topic and what areas need additional research. While scientific statements and guidance documents inform the development of formal guidelines, they do not make treatment recommendations. American Heart Association guidelines provide the Association’s official clinical practice recommendations.
Wearing PPE During CPR continues to be required

The UI Health Care’s top priority is Safety. Recently, the American Heart Association (AHA) released new guidance recommending that chest compressions or defibrillation should not be delayed for retrieval and application of a mask or face covering, for either the patient or provider.
This new guidance stems from recent observations that survival outcomes following cardiac arrest have worsened during the pandemic. This decline in survival has been attributed to multiple factors, including delays in initiating CPR due to donning personal protective equipment (PPE), and rescuer fatigue during CPR from PPE.
UI Health Care employees are required to wear a medical-grade mask at all times while in our facilities, unless they’re alone in a private office or when eating/drinking.
We believe the new guidance from the AHA has the potential to expose health care workers. Therefore, UI Health Care will maintain its current guidance that standard precautions with universal masking be followed during all patient care, with the addition of respiratory protection (N95s) during CPR.
Our decision was made after discussion with many of our experts and serves as the latest example of UI Health Care’s commitment to maintaining a safe environment for all patients, visitors, and staff.
Dec, 2021

Food and Drinks Safety Tips During Holiday Season
Prevent Food Poisoning During the Holidays
Feasting with family is part of many holiday celebrations. Follow these tips to help prevent food poisoning, or foodborne illness, during the holidays.
- Keep foods separated. Keep meat, chicken, turkey, seafood, and eggs separate from all other foods at the grocery store and in the refrigerator. Prevent juices from meat, chicken, turkey, and seafood from dripping or leaking onto other foods by keeping them in containers or sealed plastic bags. Store eggs in their original carton in the main compartment of the refrigerator.
- Cook food thoroughly. Meat, chicken, turkey, seafood, and eggs can carry germs that cause food poisoning. Use a food thermometer to ensure these foods have been cooked to a safe internal temperature. Roasts, chops, steaks, and fresh ham should rest for 3 minutes after you remove them from the oven or grill.
- Keep food out of the “danger zone.” Bacteria can grow rapidly in the danger zone between 40°F and 140°F. After food is prepared, keep hot food hot and cold food cold. Refrigerate or freeze any perishable food within 2 hours (1 hour if food is exposed to temperatures above 90°F, such as in a hot car). The temperature in your refrigerator should be set at or below 40°F and the freezer at or below 0°F.
- Use pasteurized eggs for dishes containing raw eggs. Salmonella and other harmful germs can live on both the outside and inside of normal-looking eggs. Many holiday favorites contain raw eggs, including eggnog, tiramisu, hollandaise sauce, and Caesar dressing. Always use pasteurized eggs when making these and other foods made with raw eggs.
- Do not eat raw dough or batter. Dough and batter made with flour or eggs can contain harmful germs, such as E. coli and Salmonella. Do not taste or eat raw dough or batter that is meant to be baked or cooked. This includes dough or batter for cookies, cakes, pies, biscuits, pancakes, tortillas, pizza, or crafts. Do not let children taste raw dough or batter or play with dough at home or in restaurants. Some companies and stores offer edible cookie dough that uses heat-treated flour and pasteurized eggs or no eggs. Read the label carefully to make sure the dough is meant to be eaten without baking or cooking.
- Thaw your turkey safely. Thaw turkey in the refrigerator, in a sink of cold water (change the water every 30 minutes), or in the microwave. Avoid thawing foods on the counter. A turkey must thaw at a safe temperature to prevent harmful germs from growing rapidly.
- Wash your hands. Wash your hands with soap and water during these key times when you are likely to get and spread germs:
- Before, during, and after preparing food
- Before eating food
- After handling pet food or pet treats or touching pets
- After using the toilet
- After changing diapers or cleaning up a child who has used the toilet
- After touching garbage
- Before and after caring for someone who is sick
- Before and after treating a cut or wound
- After blowing your nose, coughing, or sneezing
Holiday Food and Beverages for Pregnant
Pregnant women are at increased risk of food poisoning, so take extra care if you’re pregnant or preparing food for someone who is.
- Do not eat or drink raw or unpasteurized milk and products made with it, such as soft cheeses. They can contain harmful germs, including Listeria. Do not eat soft cheeses such as queso fresco Brie, Camembert, feta, goat cheese, or blue-veined cheese if they are made from raw or unpasteurized milk.
- Be aware that cheeses made from pasteurized milk, such as queso fresco, also have caused Listeria infections, most likely because they were contaminated during cheese-making.
- Processed cheeses, cream cheese, mozzarella, and hard cheeses are safer choices.
- Don’t drink raw or unpasteurized juice and ciderexternal icon.
- Be careful with seafoodexternal icon. Do not eat smoked seafood that was sold refrigerated unless it is in a cooked dish, such as a casserole. Instead, choose shelf-stable smoked seafood in pouches or cans that do not need refrigeration.
- Avoid certain holiday beverages. Drinking any type of alcohol can affect your baby’s growth and development and cause fetal alcohol spectrum disorders. Don’t drink holiday punches and eggnogs that contain alcohol. Avoid eggnog entirely unless you know it doesn’t contain alcohol and is pasteurized or made with pasteurized eggs and milk.
The Myths about CPR and are They True?

CPR is short for cardiopulmonary resuscitation. It is an emergency procedure in which rescue breathing and chest compressions are combined. For example, it can save a life of a person who stopped breathing or whose heart stopped beating.
The procedure itself is not simple, but still, the fact is that with proper training, children as young as nine can learn it and apply it. And statistics show that providing CPR to a victim before professional medical help arrives significantly increases the chances of survival.
So why isn’t this skill familiar to more people? Maybe the myths around CPR are to blame. In the following lines, we examine the greatest among them and if there is any truth behind them.
If you do CPR in the wrong way you can make the situation worse
Witnessing a person in a life-threatening situation is never easy, whether they are strangers or not. Many people, especially if they are just bystanders, will think: “I do not want to get involved because I might hurt this person even more.”
However, what you should keep in mind is that when a heart or breath stops, vital organs start dying very quickly. And it pretty much does not get any worse than death. So, you should try to help. Make sure you call the ambulance immediately because the dispatcher will help you with the procedure, too.
Only professionals can do CPR right
Most people have only seen CPR in movies and on TV. And there, those providing it are usually policemen, agents, firefighters, lifeguards, EMTs, nurses, and other everyday superheroes. So it makes sense then that it is commonly believed this procedure can only be done by trained professionals.
But, as we already mentioned, while not simple, the procedure is simple enough to be taught to children above the age of nine. In addition, the courses do not take much of your time.
Having done this sort of training also busts the previous myths because it gives you the confidence to do it right and helps you gain control of an emergency. All this increases the chances of survival for the victim, which is the ultimate goal.
There is no CPR without mouth-to-mouth
Another myth about CPR we probably owe to the movies and TV is the belief that CPR cannot be done without mouth-to-mouth. With this in mind, many people will give up on learning it or applying it, even if it is for their loved ones.
But in reality, a procedure called Hands-only CPR is much more common. It includes chest compressions, and statistics show that, when done correctly, they are enough. Rescue breaths, commonly known as mouth-to-mouth, should be done by professionals using an appropriate mask.
My loved ones are healthy so I will never need to use my CPR training
Most people seem to think that causes for a heart to stop or the inability to breathe are solemnly connected to serious diseases. The truth is, however, that it can be accidents that cause them, like drowning or electrocution.
We can never know when a friend or a family member can fall victim to a life-threatening accident. And unfortunately, someone’s health can get worse suddenly, so in reality, you never know when you might need to use CPR.
Another thing statistics suggest is that the person in need of CPR is more often some we care about, rather than someone on the street we never met before. So, we can think we will not need it, but reality proves otherwise.
CPR is only about saving a life
Cardiopulmonary resuscitation is necessary to save a life and we will not argue with this fact. But, most people have the misconception that that is all there is to it.
The fact is, however, that during a cardiac arrest, not enough oxygen arrives in the brain. This causes brain cell death, whose consequence is irreversible neurological damage. By applying CPR, the rescuers make sure oxygen is supplied to the brain, minimizing the risk of damage.
In a nutshell
To put it simply, one more time, CPR can save lives. This is why it is important to educate people about it, to make them understand how crucial it can be, and work our a way to eventually make it a part of every school’s curriculum. Only proper education can stop people from spreading and believing in myths.
First Support CPR and First Aid Training offers CPR classes in San Jose. For inquiries you can email us at info@firstsupportcpr.com or call us at 408-475-7724
AHA Updates CPR Guidelines for Patients With COVID-19
An updated American Heart Association (AHA) guidance on cardiopulmonary resuscitation (CPR) for patients with suspected or confirmed COVID-19 states that the risk of death to the patient from withholding or delaying treatment for cardiac arrest is extremely high, while the risk of infection and serious disease for the provider is comparably much lower, particularly in providers receiving recommended COVID-19 vaccine doses and wearing appropriate personal protective equipment (PPE).
“The guidelines appropriately evolved as we learned more about COVID-19 and its spread,” commented Lamont Hunter, MPH, PA-C, president of the Society of Emergency Medicine Physician Assistants (SEMPA) and director of Emergency Medicine Advanced Practice Providers at Cottage Health, Santa Barbara, CA. “These guidelines are useful for PAs and [nurse practitioners] working in emergency medicine and EMS and should serve as a reminder that high-quality CPR should not be delayed for those with suspected or confirmed COVID-19,” said Mr Hunter, who was not involved in the development of the AHA guidance.

The AHA guidance and collaborating organizations released their first interim guidance for the resuscitation of patients with suspected or confirmed COVID-19 in April 2020. This guidance was updated based on updated AHA CPR guidelines released in October 2020, increased understanding of SARS-CoV-2 transmissibility, more stable access to PPE, and COVID-19 vaccination.
In the latest guidelines, the AHA introduces updated COVID-19 resuscitation algorithms based on the 2020 AHA Guidelines for CPR and emergency cardiovascular care and includes a COVID-19 maternal cardiac arrest algorithm. There is a new emphasis on providing chest compressions and defibrillation without delay, and added insight about potential aerosol-generating procedures (AGPs) and when specific PPE should be used (Table).
Highlights of 2021 Interim Guidelines on Cardiac Life Support in Patients with COVID-19
| Survival outcomes for cardiac arrests have worsened since the start of the COVID-19 pandemic |
| Quality care for cardiac arrests requires rapid initiation of chest compressions. This likely carries a low risk of SARS-CoV-2 transmission to the compressor. |
| For witnessed sudden cardiac arrests, chests compressions should be initiated immediately. Providers should not delay chest compressions to put on PPE or place face covering on patients. For pediatric patients, ventilations should be prioritized. |
| Providers wearing appropriate PPE should replace providers without sufficient PPE. For aerosol-generating procedures, appropriate PPE includes N95 masks with eye protection or positive-airway pressure respirators, gloves, and gowns. |
| For agonal breathing, consider passive oxygenation overlaid with a surgical face mask (if available) until a bag-mask device or HEPA-filtered device can be applied |
| Defibrillation should be performed as soon as indicated, and should not be delayed to put on masks or other PPE |
| HEPA filters should be securely attached along the exhalation ports of any ventilation devices. Low-dead space viral filters or heat and moisture exchanging filters with >99.99% viral filtration efficiency can be installed between the ventilation device and the airway as an alternative. |
| Video laryngoscopy and mechanical compression devices may be considered in institutions where they are available and personnel are already trained |
| Advanced care directives and goals of care should be discussed with all patients with suspected or confirmed COVID-19 when they arrive at the hospital and following any significant changes in clinical status. Health care providers should commit to ethical and evidence-based organizational policies when making decisions related to initiating and continuing resuscitation. |
| Newborn babies are unlikely to spread COVID-19, regardless of their mothers’ COVID-19 status; however, maternal respiratory secretions have the potential to transmit SARS-CoV-2 |
Frequently Asked Questions about Hands Only CPR
How do you know if it’s primary cardiac arrest?
- The person is fine one moment and you suddenly see or hear them collapse.
- You then check for responsiveness by “shaking and shouting” (are you alright?) and rub the sternum with your knuckles. This helps to determine whether the person had some other reason for the event or if they are indeed in cardiac arrest. If you have no response you should assume that the person has experienced cardiac arrest.
- Tell someone to call 911 or make the call yourself. You need to get emergency responders on their way as soon as possible.
- Start chest compressions.
Just do your best. If you do nothing, the person is likely to die. Studies have shown that there is almost no chance that you will hurt the person. While it is rare that a rib will be broken during CPR, doctors are able to repair broken ribs, but they cannot repair death.
Is this the same as a heart attack?
No. In the case of a heart attack, blood flow through one of the coronary arteries becomes blocked. Remember, time is heart muscle. To preserve heart muscle, it’s important to understand early heart attack symptoms:
- Chest discomfort. The discomfort lasts for more than a few minutes or it may go away and come back. The discomfort may feel like pressure, squeezing, fullness, or pain.
- Discomfort in other areas of the upper body. This may include pain or discomfort in one or both arms, the back, neck, jaw, or upper stomach.
- Shortness of breath may occur with or before chest discomfort.
- Other symptoms may include breaking out in a cold sweat, nausea, dizziness or light-headedness, “feeling of impending doom,” weakness/fatigue.
- Women are different than men and not all symptoms of a heart attack are universal. Please check the following for more information:
If this happens to you or you witness someone who exhibits these signs: call 911.
Should I stop compressions if the victim gasps?
No! Gasping is a sign of cardiac arrest and often occurs for a while soon after the arrest and will continue when effective compressions are being delivered. It is NOT an indication of recovery. Continue chest compressions until paramedics arrive; gasping is a sign you are doing a good job.
What if I get tired during chest compressions?
Chest compressions are hard work and after 100 chest compressions or if you become fatigued, it is recommended that you switch chest comrpessions with someone nearby. To transfer chest compressions effectively, there must be less than a 10 second delay when trading off.
Can you damage someone’s heart if you perform CPR while it is beating?
The physicians and scientists at the Sarver Heart Center, have found that the old saying “Never perform CPR on beating heart” is not valid. According to these professionals, the chances that a bystander could harm a person by pressing on their chest are slim to none, even if the heart is working normally. Therefore, they recommend following the “Better safe than sorry” approach and begin chest compressions. It is better to perform a few unnecessary chest compressions for someone with a beating heart, rather than withhold chest compressions and circulation from someone in cardiac arrest.
Why don’t you check for a pulse?
We do NOT recommend that lay public rescuers waste time trying to assess for a palpable pulse. During Dr. Kern’s tenure as AHA National ACLS Chairman, the AHA came to the same conclusion. Public lay rescuers cannot reliably detect the absence of a pulse in a timely fashion, hence in the 2000 and 2005 AHA CPR Guidelines (Circulation 2005; 112(24): IV-3), this requirement was removed.
Studies have also shown that even if a person manages to locate the correct spot for detecting a pulse, there is a high chance that the pulse they may detect is their own, especially considering heightened stress levels in such situations. Rather than wasting time trying to detect a pulse that may or may not be the victim’s own pulse, it is better to get perfusion to the brain by continuous chest compressions.
The correct response to a witnessed cardiac arrest is to:
- Check for responsiveness (shake and shout).
- IF NO RESPONSE, call for help (“911”) or ask someone else to call.
- Begin uninterrupted forceful continuous chest compressions immediately.
- Call for an AED if one is nearby and available.
Don’t you need to check the airway first?
If you see or hear someone suddenly collapse and they did not show any sign of choking, you don’t have to worry about checking the airway. Assume it’s a sudden cardiac arrest and follow the 3 Cs: Check for responsiveness (shake and shout), Call 911 and Compress at a rate of 100 per minute, about 2 inches deep. If by some chance an object is lodged in the throat, effective compressions likely will dislodge the object, similarly to the way abdominal thrusts (the Heimlich Maneuver) dislodges objects.
Do I have to remove a person’s clothes to do Chest-Compression-Only CPR or only when using an AED?
It is not necessary to remove a patient’s clothing in order to do chest-compression-only CPR. However, if an AED is available, turn on the device and follow the instructions, which state to “remove patient’s clothing.” Defibrillator pads must be placed directly on the patient’s skin in order for the electrical current to be conducted.
How does the victim get oxygen with Chest-Compression-Only CPR?
When someone’s heart has stopped, blood is no longer circulated through the body and therefore hardly any of the oxygen in the blood is used. The person was breathing normally only seconds ago, so their blood contains enough oxygen to tide them over for several minutes. However, it is crucial to deliver blood and oxygen to the brain by performing chest compressions continuously.
Remember: Your hands become their heart and each chest compression becomes their heart beat. Performing adequate chest compressions also increases the likelihood that the patient will gasp or continue to gasp, allowing the lungs to obtain fresh oxygen.
What if the person has an ICD or a pacemaker?
Fortunately, the answer is short and simple: Don’t worry about it. If the person in cardiac arrest has an ICD, the ICD is not functioning properly, since its purpose is to PREVENT cardiac arrest from happening. Pacemakers have a different function, but the answer remains the same, continuous chest compressions should be performed. It is important to recognize that someone in cardiac arrest is either dead or will be dead unless you intervene.
What if the person recently underwent open heart surgery, couldn’t this crack the chest bone?
The key message here is that you cannot do more damage. It is important to recognize that someone in cardiac arrest is dying or will soon be dead unless you intervene. Since this person’s heart is no longer functioning properly on its own, your compressions are doing the heart’s job. Yes, if the person has had recent surgery, you might break the wires in their breast bone. However, the alternative is death.
Can I be held liable for performing Chest-Compression Only CPR?
The Good Samaritan law protects bystanders and their actions when they decide to help someone in an emergency. There is some form of the Good Samaritan Law in all states of the U.S. Chest-Compression-Only CPR and conventional CPR are both covered under the Good Samaritan Law. It does not matter whether you are certified or not but remember to always respect the patient.
Will chest compressions alone bring the person back or restart the heart?
It is highly unlikely that chest compressions alone will result in recovery. However, by maintaining uninterrupted chest compressions, you can dramatically increase the chance of survival by maintaining the patient’s heart in a state that increase the likelihood that shocks from a defibrillator, administered through bystanders using an Automated External Defibrillator (AED), or administered by paramedics will result in survival.
Can this method be used in all arrests?
For unresponsiveness in young children (age 8 or under), drowning cases, or drug overdoses, follow conventional CPR guidelines (30 chest compressions followed by two mouth-to-mouth ventilations). This is because in infants or children, respiratory arrest is more common than primary cardiac arrest. However, even in these cases, Chest-Compression-Only CPR is better than doing nothing. To learn conventional CPR, a certification class is recommended.
CPR Classes in San Jose

First Support CPR and First Aid Training offers CPR Classes in San Jose California. We offer BLS Provider, First Aid, First Aid CPR AED, CPR AED and Pediatric First Aid CPR AED. Our classes are every Tuesday and Friday at 7:15 PM or if you wish, we can schedule a special class for you with a minimum of 3 persons. We are American Heart Association Authorized Training Center. After taking the CPR class, students will receive the certification card right away through email. CPR Classes take place at our own facilities rather than in the downtown area where students are required to park in the garage where they would have to pay for parking. Students shouldn’t have to pay for parking for a class that they are already paying for. Therefore parking is free when you take a CPR Class with us.
Learning how to save a life is important and everyone should know how to do it.
If you have any question, you can call us at (408) 475-7724 or email us at info@firstsupportcpr.com
© 2025 First Support CPR & First Aid Training. All rights reserved.
