How do you know if it’s primary cardiac arrest?
- The person is fine one moment and you suddenly see or hear them collapse.
- You then check for responsiveness by “shaking and shouting” (are you alright?) and rub the sternum with your knuckles. This helps to determine whether the person had some other reason for the event or if they are indeed in cardiac arrest. If you have no response you should assume that the person has experienced cardiac arrest.
- Tell someone to call 911 or make the call yourself. You need to get emergency responders on their way as soon as possible.
- Start chest compressions.
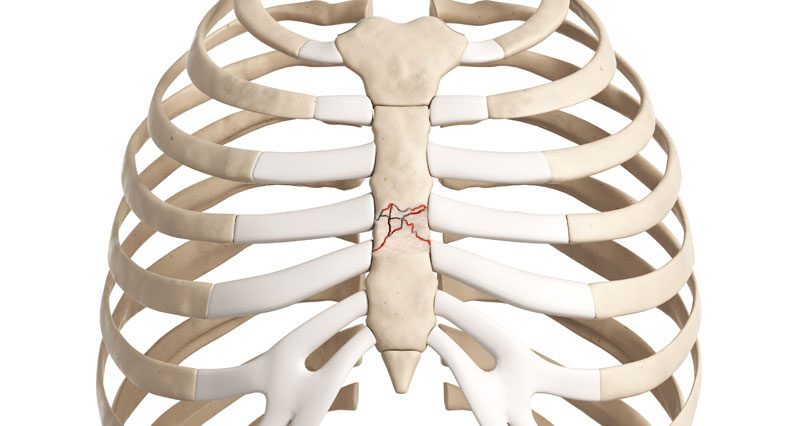
Just do your best. If you do nothing, the person is likely to die. Studies have shown that there is almost no chance that you will hurt the person. While it is rare that a rib will be broken during CPR, doctors are able to repair broken ribs, but they cannot repair death.
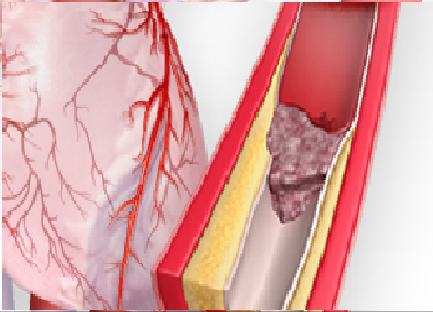
Is this the same as a heart attack?
No. In the case of a heart attack, blood flow through one of the coronary arteries becomes blocked. Remember, time is heart muscle. To preserve heart muscle, it’s important to understand early heart attack symptoms:
- Chest discomfort. The discomfort lasts for more than a few minutes or it may go away and come back. The discomfort may feel like pressure, squeezing, fullness, or pain.
- Discomfort in other areas of the upper body. This may include pain or discomfort in one or both arms, the back, neck, jaw, or upper stomach.
- Shortness of breath may occur with or before chest discomfort.
- Other symptoms may include breaking out in a cold sweat, nausea, dizziness or light-headedness, “feeling of impending doom,” weakness/fatigue.
- Women are different than men and not all symptoms of a heart attack are universal. Please check the following for more information:
If this happens to you or you witness someone who exhibits these signs: call 911.
Should I stop compressions if the victim gasps?
No! Gasping is a sign of cardiac arrest and often occurs for a while soon after the arrest and will continue when effective compressions are being delivered. It is NOT an indication of recovery. Continue chest compressions until paramedics arrive; gasping is a sign you are doing a good job.
What if I get tired during chest compressions?
Chest compressions are hard work and after 100 chest compressions or if you become fatigued, it is recommended that you switch chest comrpessions with someone nearby. To transfer chest compressions effectively, there must be less than a 10 second delay when trading off.
Can you damage someone’s heart if you perform CPR while it is beating?
The physicians and scientists at the Sarver Heart Center, have found that the old saying “Never perform CPR on beating heart” is not valid. According to these professionals, the chances that a bystander could harm a person by pressing on their chest are slim to none, even if the heart is working normally. Therefore, they recommend following the “Better safe than sorry” approach and begin chest compressions. It is better to perform a few unnecessary chest compressions for someone with a beating heart, rather than withhold chest compressions and circulation from someone in cardiac arrest.
Why don’t you check for a pulse?
We do NOT recommend that lay public rescuers waste time trying to assess for a palpable pulse. During Dr. Kern’s tenure as AHA National ACLS Chairman, the AHA came to the same conclusion. Public lay rescuers cannot reliably detect the absence of a pulse in a timely fashion, hence in the 2000 and 2005 AHA CPR Guidelines (Circulation 2005; 112(24): IV-3), this requirement was removed.
Studies have also shown that even if a person manages to locate the correct spot for detecting a pulse, there is a high chance that the pulse they may detect is their own, especially considering heightened stress levels in such situations. Rather than wasting time trying to detect a pulse that may or may not be the victim’s own pulse, it is better to get perfusion to the brain by continuous chest compressions.
The correct response to a witnessed cardiac arrest is to:
- Check for responsiveness (shake and shout).
- IF NO RESPONSE, call for help (“911”) or ask someone else to call.
- Begin uninterrupted forceful continuous chest compressions immediately.
- Call for an AED if one is nearby and available.
Don’t you need to check the airway first?
If you see or hear someone suddenly collapse and they did not show any sign of choking, you don’t have to worry about checking the airway. Assume it’s a sudden cardiac arrest and follow the 3 Cs: Check for responsiveness (shake and shout), Call 911 and Compress at a rate of 100 per minute, about 2 inches deep. If by some chance an object is lodged in the throat, effective compressions likely will dislodge the object, similarly to the way abdominal thrusts (the Heimlich Maneuver) dislodges objects.
Do I have to remove a person’s clothes to do Chest-Compression-Only CPR or only when using an AED?
It is not necessary to remove a patient’s clothing in order to do chest-compression-only CPR. However, if an AED is available, turn on the device and follow the instructions, which state to “remove patient’s clothing.” Defibrillator pads must be placed directly on the patient’s skin in order for the electrical current to be conducted.
How does the victim get oxygen with Chest-Compression-Only CPR?
When someone’s heart has stopped, blood is no longer circulated through the body and therefore hardly any of the oxygen in the blood is used. The person was breathing normally only seconds ago, so their blood contains enough oxygen to tide them over for several minutes. However, it is crucial to deliver blood and oxygen to the brain by performing chest compressions continuously.
Remember: Your hands become their heart and each chest compression becomes their heart beat. Performing adequate chest compressions also increases the likelihood that the patient will gasp or continue to gasp, allowing the lungs to obtain fresh oxygen.
What if the person has an ICD or a pacemaker?
Fortunately, the answer is short and simple: Don’t worry about it. If the person in cardiac arrest has an ICD, the ICD is not functioning properly, since its purpose is to PREVENT cardiac arrest from happening. Pacemakers have a different function, but the answer remains the same, continuous chest compressions should be performed. It is important to recognize that someone in cardiac arrest is either dead or will be dead unless you intervene.
What if the person recently underwent open heart surgery, couldn’t this crack the chest bone?
The key message here is that you cannot do more damage. It is important to recognize that someone in cardiac arrest is dying or will soon be dead unless you intervene. Since this person’s heart is no longer functioning properly on its own, your compressions are doing the heart’s job. Yes, if the person has had recent surgery, you might break the wires in their breast bone. However, the alternative is death.
Can I be held liable for performing Chest-Compression Only CPR?
The Good Samaritan law protects bystanders and their actions when they decide to help someone in an emergency. There is some form of the Good Samaritan Law in all states of the U.S. Chest-Compression-Only CPR and conventional CPR are both covered under the Good Samaritan Law. It does not matter whether you are certified or not but remember to always respect the patient.
Will chest compressions alone bring the person back or restart the heart?
It is highly unlikely that chest compressions alone will result in recovery. However, by maintaining uninterrupted chest compressions, you can dramatically increase the chance of survival by maintaining the patient’s heart in a state that increase the likelihood that shocks from a defibrillator, administered through bystanders using an Automated External Defibrillator (AED), or administered by paramedics will result in survival.
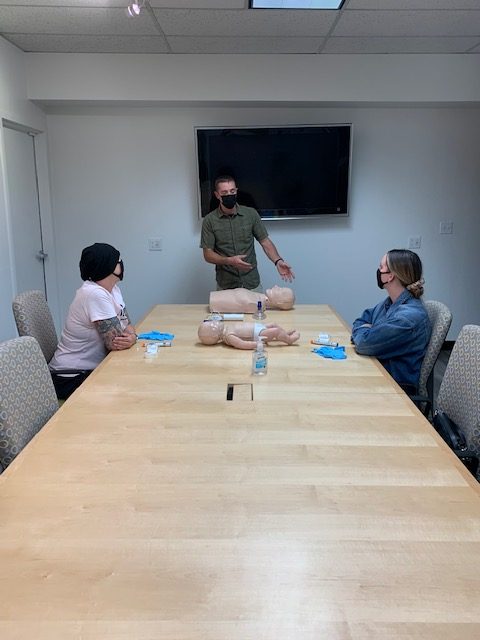
Can this method be used in all arrests?
For unresponsiveness in young children (age 8 or under), drowning cases, or drug overdoses, follow conventional CPR guidelines (30 chest compressions followed by two mouth-to-mouth ventilations). This is because in infants or children, respiratory arrest is more common than primary cardiac arrest. However, even in these cases, Chest-Compression-Only CPR is better than doing nothing. To learn conventional CPR, a certification class is recommended.